If you are suffering from dental pain, infection or inflammation of the dental pulp, endodontic treatment, or root canal therapy, may be necessary to preserve your oral health. If you’re wondering about the nature of this treatment, how it works and its benefits, you’ve come to the right place. Then you’ve come to the right place. In this article, we’ll provide you with essential information on endodontics, how endodontic treatment works, the conditions it can treat, and preventive advice for the dental pulp. We will also look at the costs and financial coverage of this procedure. Endodontics is a specialised branch of dentistry that requires expertise and experience. We explain why consulting an endodontist, a professional specialising in this field, is crucial if you are to benefit from the most appropriate care. Join us on this in-depth exploration of endodontics to decipher its challenges and solutions. If you have any questions or require personal advice, please do not hesitate to contact us.
What is endodontics?
Definition and objectives
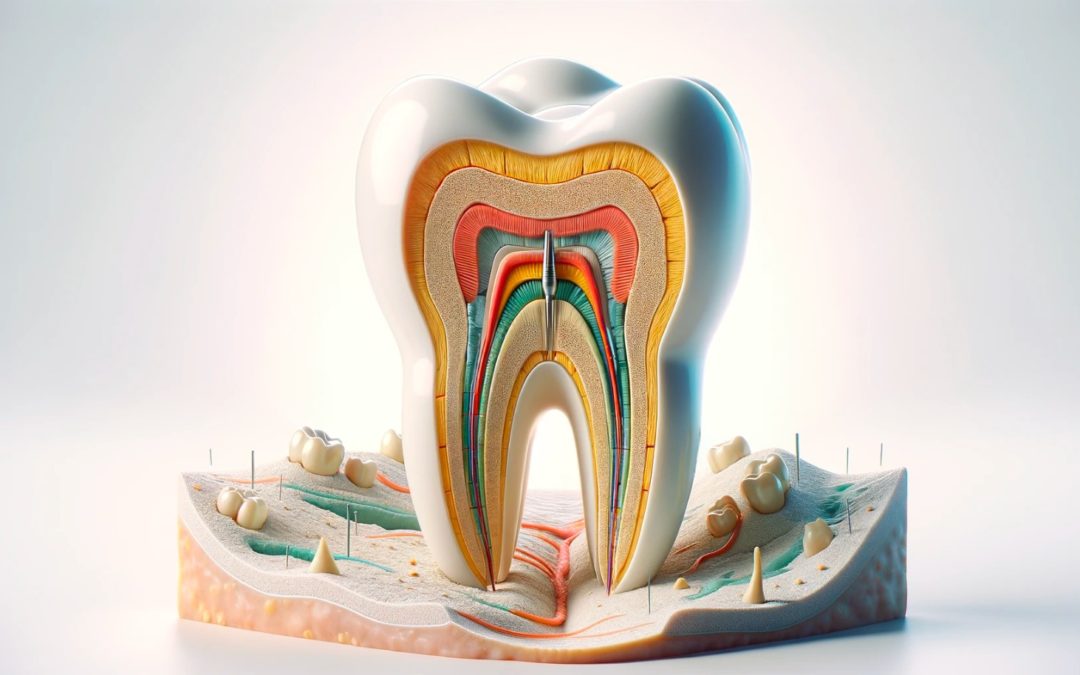
Endodontics is a speciality of dentistry that focuses on the treatment of the dental pulp and the tissues surrounding the root of the tooth. It is particularly interested in the soft tissue inside the tooth, made up of nerves, blood vessels and connective tissue. Its main aim is to treat diseases and lesions of the pulp, as well as problems relating to the dental root. The most common endodontic procedure is devitalisation, which involves the removal of infected or damaged pulp followed by the sealing of the root canal.
The importance of healthy pulp
Healthy dental pulp is crucial to the overall well-being of the tooth and mouth. It plays a key role in the development, nourishment and receptivity of the tooth, enabling it to respond to various external stimuli such as temperature and pressure. Exposure to deep decay, direct impact or repeated dental procedures can lead to inflammation or infection of the pulp, causing pain and other complications. Left untreated, the pulp can deteriorate, leading to tooth loss or more serious infections.
Common symptoms requiring endodontic treatment
Here are some signs indicating the need for endodontic treatment:
- Constant or episodic pain in a tooth, sensitive to temperature variations or when chewing.
- Swelling or redness of the gums around the tooth concerned.
- Change in colour of the tooth to a dark or grey shade.
- Presence of an abscess or discharge of pus near the tooth root.
- Increased mobility or sensitivity of the tooth.
- Existence of a fracture or fissure exposing the dental pulp.
The Endodontic Treatment Process
Assessment and diagnosis
The first step before undertaking endodontic treatment is a thorough assessment of the condition of the tooth and the pulp. This assessment is carried out by the dentist or endodontist, who makes a detailed examination of the tooth, takes X-rays and tests its sensitivity. He will also look for any signs of infection or inflammation, such as swelling, redness or abscesses. Based on these observations, a precise diagnosis is made and a suitable treatment plan proposed.
Stages of root canal treatment
Root canal treatment is generally carried out over one or two sessions, depending on the complexity of the situation. The main stages include :
- Applying local anaesthetic around the tooth and adjacent tissues.
- Isolating the tooth with a rubber dam to prevent bacterial contamination from saliva.
- Careful opening of the upper part of the tooth to gain access to the pulp.
- Removal of infected or damaged pulp using special instruments known as endodontic files.
- Cleaning and disinfection of the root canals with antiseptic solutions, typically sodium hypochlorite or calcium hydroxide.
- Widening and shaping the canals to allow effective obturation.
- Filling the canals with a biocompatible material, such as gutta-percha, to fill the empty space and seal the tooth securely.
- Closing the tooth with a temporary or permanent material, such as composite resin or a crown, to protect it.
After treatment: practical advice
Following root canal treatment, it is important to follow certain tips to promote healing and maintain the health of the treated tooth:
- Avoid chewing or stressing the treated tooth until it has been fully restored.
- Adopt rigorous oral hygiene, brushing twice a day and using dental floss.
- See your dentist or endodontist regularly to monitor the progress of your tooth and prevent any complications.
- Immediately report any abnormal symptoms, such as persistent pain, swelling, fever or a bitter taste sensation.
- Consulting patient associations and specialized forums
Pathologies Treatable by Endodontics
Pulpitis and its implications
Pulpitis is an inflammation of the dental pulp, which can present different degrees: acute or chronic, reversible or irreversible. This condition is caused by various irritating factors, such as bacteria, temperature variations, physical trauma or the after-effects of dental restorations. It is characterised by intense pain, whether spontaneous or provoked, which can spread to the ear, temple or jaw. If left untreated, pulpitis can lead to serious complications such as necrosis (death) of the pulp, infection of the root tip (periapical infection) or periodontitis. To treat pulpitis, it is essential to remove the source of the irritation, relieve the pain and try to maintain the vitality of the dental pulp as much as possible. Treatment approaches vary depending on the condition of the pulp, ranging from conservative solutions (such as pulp capping or pulpotomy) to more radical treatments (such as devitalisation).
Pulpal necrosis
When the dental pulp dies, partially or totally, locally or extensively, it is known as pulpal necrosis. This condition usually results from irreversible destruction of the pulp cells following untreated pulpitis, direct trauma or ischaemia. Pulpal necrosis is manifested by a loss of sensitivity in the affected tooth, which may also change colour to grey or yellow. It can be a breeding ground for anaerobic bacteria in the root canals, leading to periapical infections such as abscesses, granulomas and cysts. To treat pulpal necrosis, endodontic treatment is necessary. This involves cleaning, disinfecting and sealing the root canals to eliminate the infection.
Periapical pathologies: from abscesses to desmodontitis
Periapical pathologies involve the tissues around the apex (tip) of the dental root, including the desmodont, the alveolar bone and the alveolar-dental ligament. Most of these conditions are endodontic in origin, resulting from the spread of bacteria from a necrotic pulp to the periapical area. They can be distinguished by clinical symptoms such as pain, swelling, the formation of a fistula or tooth mobility, and can be identified by specific radiological signs such as the loss of the lamina dura, a radiolucent lesion or bone resorption. There are two main types of periapical pathology: apical periodontitis, corresponding to acute or chronic inflammatory reactions, and cystic lesions, which are chronic proliferative forms. Their treatment aims to eradicate the endodontic infection, drain the abscess if necessary and promote adequate healing of the periapical area.
Conclusion
This article has taken you through the basics of endodontics, including how endodontic treatment works and the various diseases it aims to treat. You now have a better understanding of the crucial importance of pulp health, as well as the symptoms that signal the need to consult an endodontic specialist. In addition, we’ve provided you with preventive strategies to avoid problems with the dental pulp and shared details about the costs and reimbursement of endodontic treatment. We hope you find this information both useful and enlightening. If you are considering endodontic treatment, we encourage you to seek the services of a competent and experienced endodontist, who will guarantee the highest quality of care. Take good care of your smile, and we look forward to seeing you again!
FAQ
What is endodontic treatment?
Endodontic treatment is a dental procedure designed to remove infected or damaged pulp from a tooth and then fill the root canal with an impermeable material. The aim of this procedure is to save the tooth concerned, preventing its extraction and preventing secondary infections.
Does endodontics hurt?
Endodontics is a dental care procedure that involves removing infected or inflamed pulp from a tooth, followed by sealing it. Performed under local anaesthetic, endodontics is generally painless during the operation. However, it is possible to experience minor discomfort after treatment.
What is the difference between a dentist and an endodontist?
The main distinction between a dentist and an endodontist lies in their specialisation. An endodontist focuses exclusively on the internal care of the tooth – including the pulp, canal, nerves and surrounding tissues. A dentist, on the other hand, is responsible for general oral health maintenance and may refer patients to an endodontist for cases requiring special expertise.
Why is endodontics not reimbursed?
Endodontics is not fully reimbursed because the standard cost set by social security is much lower than the actual expenses of this dental procedure. Furthermore, social security is gradually reducing its coverage in the dental field, excluding certain endodontic procedures from its coverage.