Periodontology (loosening of the teeth)
Periodontitis (gum infection)
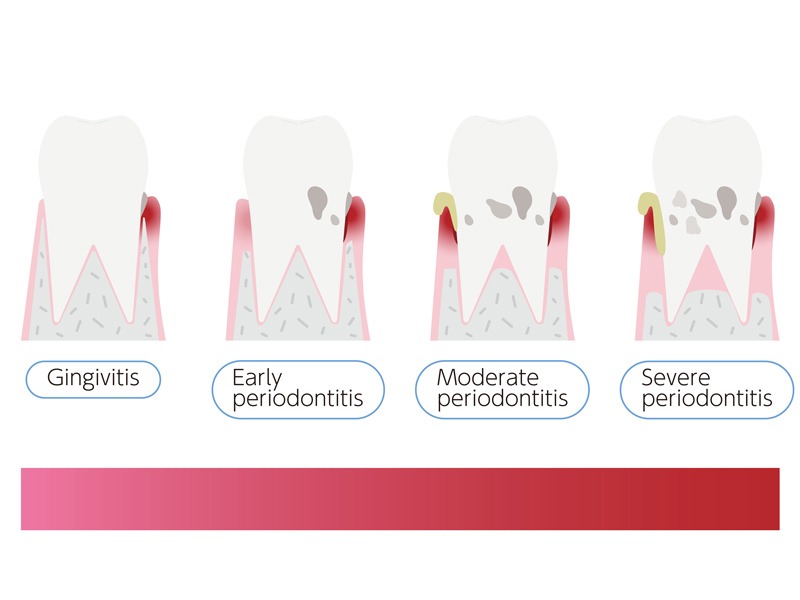
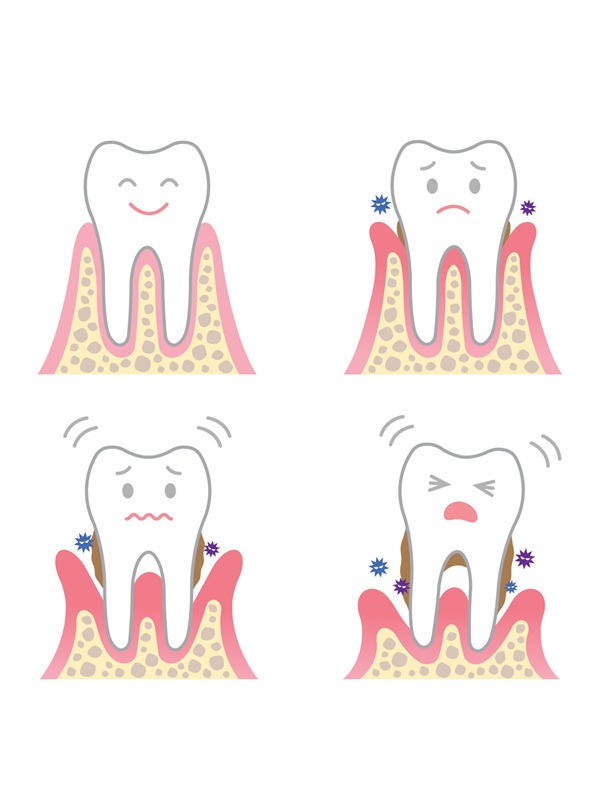
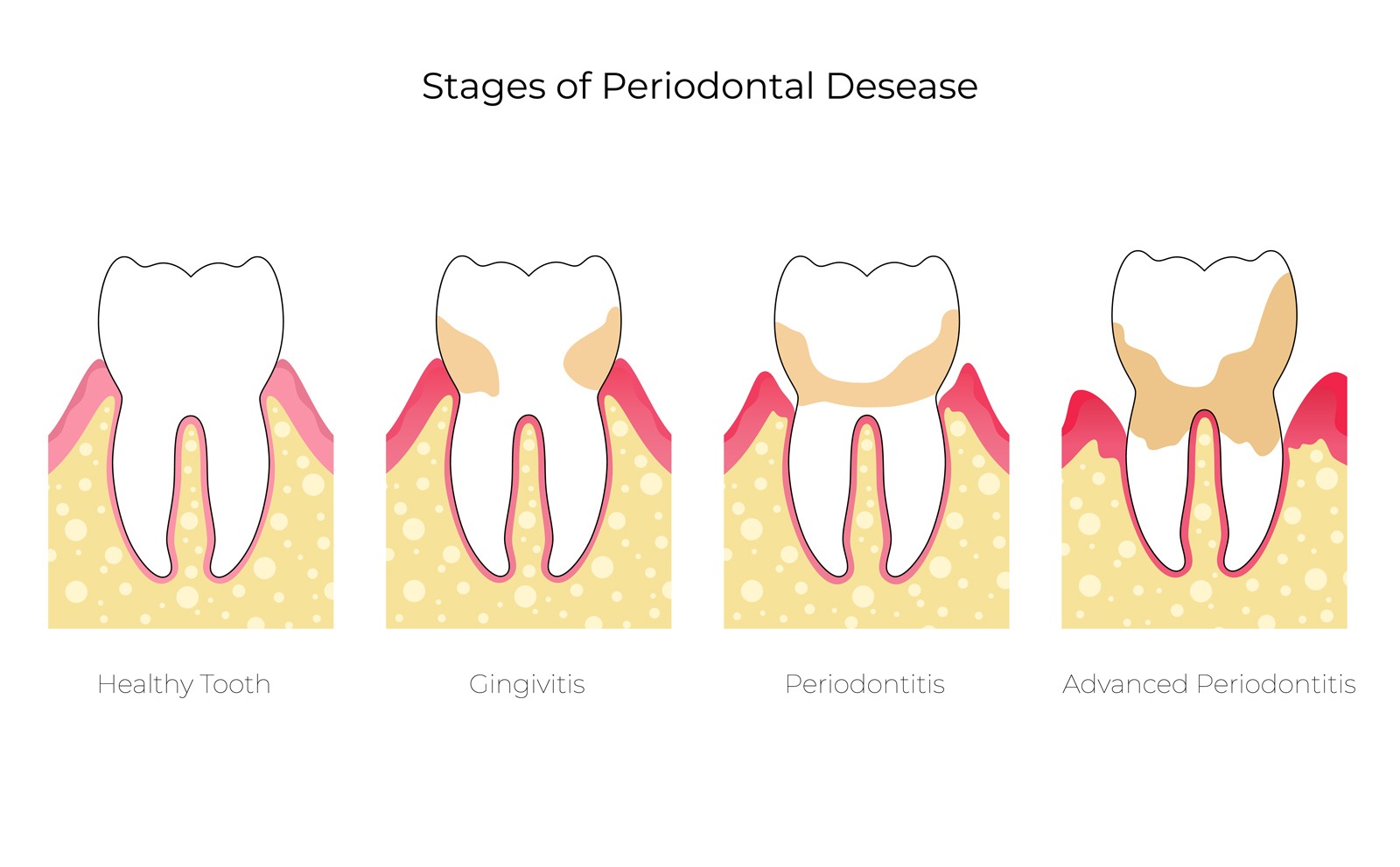
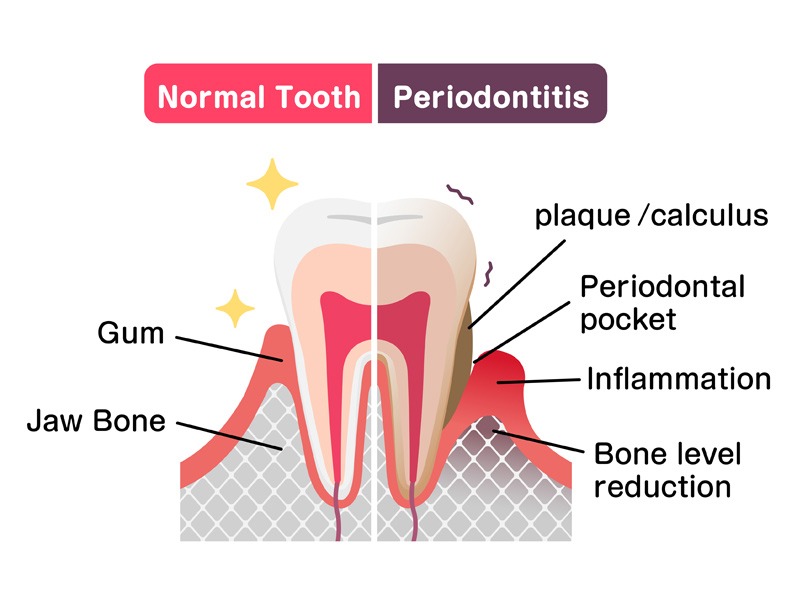
Periodontitis, or periodontal disease, is a chronic infection of the gums that causes the destruction of the bone and gums around the teeth. It is an insidious disease because it has no symptoms. It is progressive and leads to the loss of teeth. It is dangerous for the body because the bacteria that cause it can attack the heart, the kidneys or the fetus.
The cause of periodontitis
Periodontitis is caused by certain bacteria known as periodontal bacteria. Although these periodontal bacteria are naturally present in the mouth, they only become harmful when they increase considerably in number, when certain conditions are met.
This occurs when a layer of bacteria and food debris, called bacterial plaque, builds up on the teeth and remains intact, usually in hard-to-reach areas such as between the teeth.
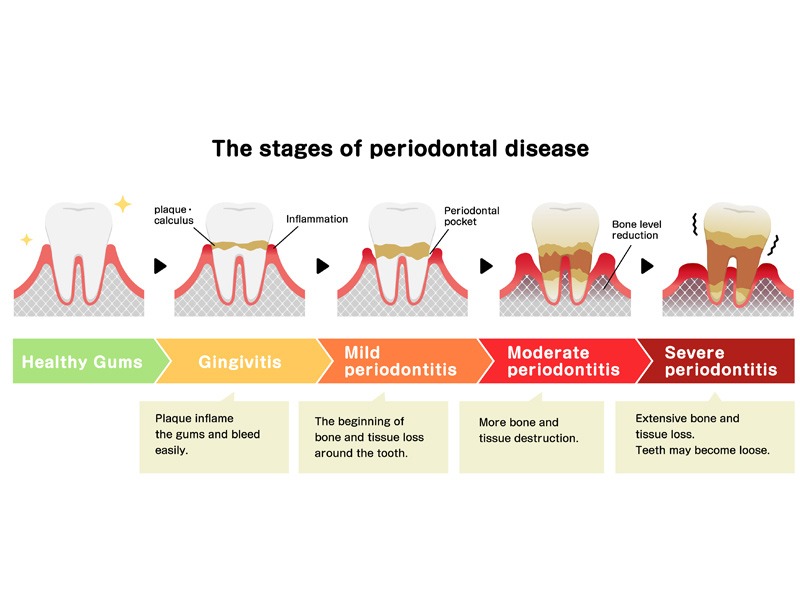
As the disease progresses, the chronic inflammation gradually leads to the destruction of the jawbone, eventually leading to tooth loss.
Nevertheless, for most people, periodontitis is a slow and progressive process that takes place over many years and can be stopped if detected and treated in time.
However, some young adults have a very active form of the disease that causes loosening and early tooth loss.
It is important to understand that without the accumulation of bacterial plaque, periodontitis will not occur.
Periodontitis is a serious pathology
When you look at it, the condition of your mouth can be seen as a mirror of the general condition of your body, and your periodontal condition can often tell you more about your health than just the condition of your gums.
Although periodontitis is always triggered by the accumulation of plaque on the teeth, diseases affecting the rest of the body, known as systemic diseases, can also weaken the support structures of our teeth.
In addition, some serious conditions are known to occur in the mouth before they appear in other parts of the body. Therefore, a qualified periodontologist may be the first to detect signs of a general disease, such as diabetes or blood disorders, when examining a patient’s mouth.
Recognizing periodontitis
Periodontitis always starts with an inflammation of the gums, known as gingivitis. This inflammation is not always easy to recognize, but one of the first signs you may notice is bleeding gums when you brush your teeth.
Gums may appear red and swollen, and you may notice a whitish layer – bacterial plaque – on the teeth.
If left untreated, gingivitis can progress to periodontitis, which often has no obvious signs to alert you. However, there are some changes that can occur over time that can alert you:

Increased bleeding of the gums (caused by brushing or eating, or sometimes spontaneous)

Bad Breath

Changes in the position of the teeth

Tooth lengthening (gingival recession)

Pain
Depistage
Often, the presence of periodontitis is not recognized by an individual until they are 40 or 50 years old, when much damage has already been done. However, a dentist should be able to detect signs of the disease at a much earlier stage during a routine examination and can monitor your periodontal condition with a specific assessment called a periodontal screening index.
Prevention of periodontitis
Fortunately, periodontal inflammation is preventable.
You can prevent the development of gingivitis and periodontitis by adopting effective oral hygiene habits and having regular professional check-ups and cleanings.
Here are the basic elements of a good oral hygiene regimen:
- clean the chewing surfaces and sides of the teeth twice a day with a toothbrush (of appropriate size and in good condition) and toothpaste
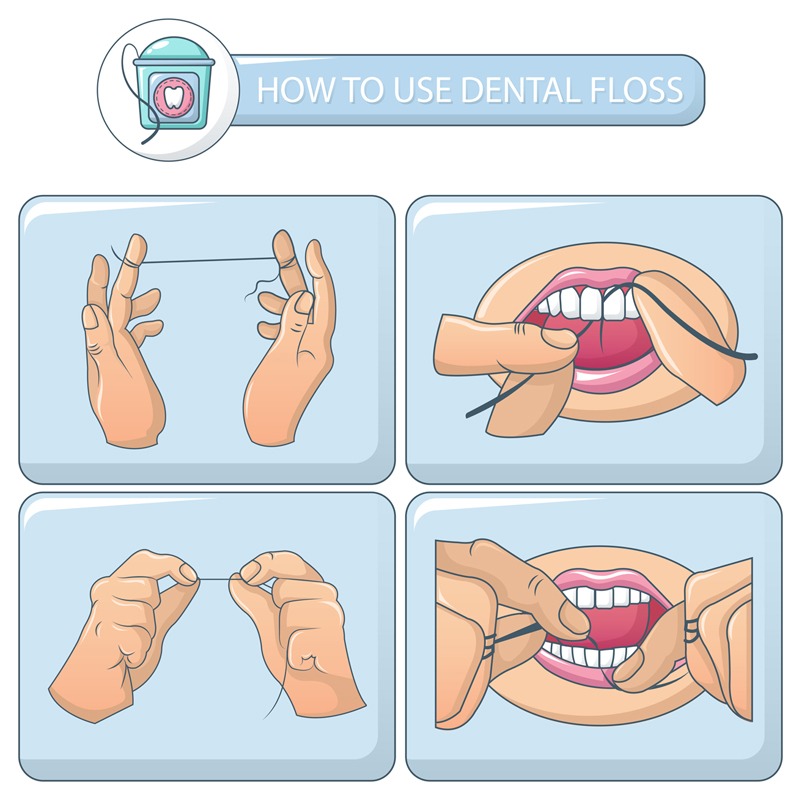
- clean the spaces between the teeth (areas that cannot be reached by the toothbrush bristles) once a day with dental floss or an interdental brush adapted to the size of the space
Floss when teeth are close together, with little or no space between them, and use the interdental brush for wider spaces.
It is important to take special care to clean crooked or crowded teeth, as well as around fillings, crowns and dentures, as plaque can easily accumulate in these restricted areas.
Antibacterial mouthwashes are a useful complement to brushing because they inhibit bacterial growth and dampen inflammatory changes. Mouthwashes are used after brushing.
If, as a result of an inadequate cleaning technique, plaque deposits remain on the teeth, they mineralize and turn into hard, fixed deposits (tartar) that can no longer be removed with a toothbrush. Your dentist or periodontologist will identify these tartar deposits during your regular dental inspection and will remove them during a professional cleaning. Once the deposits are removed, the teeth will be polished to create a smooth surface that is less likely to accumulate plaque.
The consequences of periodontitis
Periodontitis is the main cause of tooth loss. If the progression of periodontal inflammation is not stopped, the supporting structures of the teeth, including the surrounding bone, are destroyed. Teeth eventually loosen and are lost, or they must be extracted. In addition, other problems may occur in some patients, including painful abscesses, drifting of the teeth that can interfere with eating, and unsightly elongation of the teeth with exposed roots due to gum recession.
It is now recognized that untreated periodontal disease can affect overall health, such as increasing the risk of complications during pregnancy (pre-eclampsia, premature birth or low birth weight) and the risk of heart disease or diabetes.
In summary, here is a good dental hygiene sequence:
- Morning and noon:
Brushing for 2 minutes (electric brushing time), mouthwash
- Evening:
wire/brush, brushing, mouthwash
Morning and Noon
Brushing for 2 minutes (electric brushing time), mouthwash
Evening
wire/brush, brushing, mouthwash
Risk factors for periodontitis
There are a number of factors that increase the risk of developing periodontitis and that can promote its progression, such as stress or certain systemic diseases like diabetes and smoking.
Smokers are significantly more likely to develop periodontitis than non-smokers.
Periodontal treatments (e.g., gum or bone grafts, implants) are less effective in smokers than in non-smokers because of less effective healing.
In smokers, periodontitis progresses much faster, with more rapid tooth loss.
About 90% of the cases of periodontitis that do not respond to treatment are in smokers.
Treatment of periodontitis
With careful evaluation and treatment, it is usually possible to completely stop the progression of periodontitis. The key to success is to eliminate the bacterial plaque that triggers the disease process and to implement excellent oral hygiene practices.
Oral hygiene instructions and tips
The goal of the initial treatment phase is to reduce the number of bacteria in the mouth and thus decrease the level of inflammation.
Your dentist or hygienist will first explain the causes of your periodontitis and tell you exactly how to keep your teeth and gums clean. They will give you individual advice on how to use the various cleaning methods most effectively (e.g. the most appropriate tooth brushing technique, proper use of dental floss and interdental brushes).
Course of the periodontal treatment
Periodontal treatment is performed in stages; after each stage, a reassessment will determine the need to proceed to the next stage.

Professional cleaning

Antibiotic therapy

Reassessment

Corrective treatment (surgical)

Follow-up: supportive periodontal therapy

The professional cleaning consists of removing all bacterial deposits around the teeth and polishing the teeth. Depending on the progress of the periodontitis and the improvement of the gums, we can give you further instructions and perform additional cleaning during subsequent visits. The next step will be to remove all bacterial deposits and tartar lodged in the depth of the gum pockets, anchored to the surface of the roots
The professional cleaning consists of removing all bacterial deposits around the teeth and polishing the teeth. Depending on the progress of the periodontitis and the improvement of the gums, we can give you further instructions and perform additional cleaning during subsequent visits. The next step will be to remove all bacterial deposits and tartar lodged in the depth of the gum pockets, anchored to the surface of the roots

Antibiotics are sometimes prescribed to treat active or persistent gum infections that have not responded to oral hygiene measures.
Antibiotics are sometimes prescribed to treat active or persistent gum infections that have not responded to oral hygiene measures.

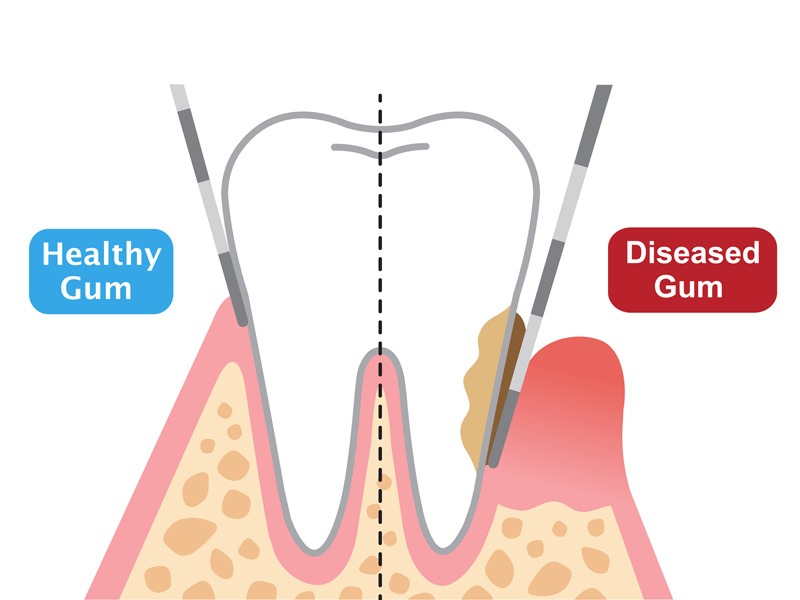
A few weeks after the initial treatment, your periodontologist will do a complete evaluation of your gums to check the results of this first phase. He or she will use a special instrument, called a periodontal probe, to record the depth of the periodontal pockets and check for bleeding gums. If periodontal pockets are still present, he or she may suggest other treatment options, including surgical corrective therapy.
A few weeks after the initial treatment, your periodontologist will do a complete evaluation of your gums to check the results of this first phase. He or she will use a special instrument, called a periodontal probe, to record the depth of the periodontal pockets and check for bleeding gums. If periodontal pockets are still present, he or she may suggest other treatment options, including surgical corrective therapy.

Sometimes a surgical procedure is necessary to remove plaque bacteria and deposits from under the gum, deep in the periodontal pockets and on the root surfaces. Since these areas are inaccessible to brushes and floss, inflammation will persist as long as bacteria can colonize them. Under local anesthesia, the gum is removed and the root surfaces are cleaned under direct vision to ensure that all bacteria are removed. Sometimes bone loss can be treated at the same time with a special regenerative treatment. At the end of the procedure, the gum is sutured back around the teeth.
Sometimes a surgical procedure is necessary to remove plaque bacteria and deposits from under the gum, deep in the periodontal pockets and on the root surfaces. Since these areas are inaccessible to brushes and floss, inflammation will persist as long as bacteria can colonize them. Under local anesthesia, the gum is removed and the root surfaces are cleaned under direct vision to ensure that all bacteria are removed. Sometimes bone loss can be treated at the same time with a special regenerative treatment. At the end of the procedure, the gum is sutured back around the teeth.

The long-term success of periodontal treatment depends on both your oral hygiene efforts and the work of the office team in providing care and evaluating you periodically. Once the first phase of treatment is complete, your dentist will need to examine the condition of your gums at regular intervals to ensure that the inflammation has been stopped. The frequency of your follow-up appointments will depend on the severity of the disease and your individual risk of disease progression. In general, follow-up visits are scheduled every 3 to 6 months.
It is important to have regular follow-up appointments to ensure that the disease process does not start again, leading to further destruction of the gums and supporting bone. If there are early signs of the disease, your dentist will be able to identify and treat them at an early stage. He or she will also give you advice on how to change your oral hygiene practices to fight inflammation.
The long-term success of periodontal treatment depends on both your oral hygiene efforts and the work of the office team in providing care and evaluating you periodically. Once the first phase of treatment is complete, your dentist will need to examine the condition of your gums at regular intervals to ensure that the inflammation has been stopped. The frequency of your follow-up appointments will depend on the severity of the disease and your individual risk of disease progression. In general, follow-up visits are scheduled every 3 to 6 months.
It is important to have regular follow-up appointments to ensure that the disease process does not start again, leading to further destruction of the gums and supporting bone. If there are early signs of the disease, your dentist will be able to identify and treat them at an early stage. He or she will also give you advice on how to change your oral hygiene practices to fight inflammation.
Other conditions that can affect periodontal health
A number of general conditions can increase your chances of developing periodontitis and potentially put you in a high-risk category. Sometimes the effects of another disease can increase your risk of gum problems (e.g., diabetes) or prescribed medications can have an adverse effect (e.g., phenytoin for epilepsy, nifedipine for hypertension).

High blood pressure
Diabetes (and over 40 years old)
Organ transplant recipients

Epilipsy

If you have high blood pressure, you should be aware of the effects that certain prescribed medications can have on the health of your gums. Knowing this can help you take steps to protect yourself from gum problems and tooth loss.
What can you do to remedy this problem?
Although blood pressure medications may be responsible for changes in the size and shape of the gums, the presence of plaque around the teeth remains the most important cause of periodontitis, as the inflammatory changes are triggered by periodontal bacteria. In addition, gum overgrowth tends to be worse in sites where bacteria accumulate easily and usually begins between the teeth. This creates a vicious cycle, as the overgrown areas then become even more difficult to clean due to the extra gum tissue. Effective plaque removal is therefore the key to limiting excessive gum growth and preventing inflammation, tissue destruction and tooth loss.
If you have high blood pressure, you should be aware of the effects that certain prescribed medications can have on the health of your gums. Knowing this can help you take steps to protect yourself from gum problems and tooth loss.
What can you do to remedy this problem?
Although blood pressure medications may be responsible for changes in the size and shape of the gums, the presence of plaque around the teeth remains the most important cause of periodontitis, as the inflammatory changes are triggered by periodontal bacteria. In addition, gum overgrowth tends to be worse in sites where bacteria accumulate easily and usually begins between the teeth. This creates a vicious cycle, as the overgrown areas then become even more difficult to clean due to the extra gum tissue. Effective plaque removal is therefore the key to limiting excessive gum growth and preventing inflammation, tissue destruction and tooth loss.
Diabetes mellitus – a condition in which the body is unable to properly control its sugar levels – is an increasingly common disease in Western countries, affecting at least 5% of the population. This is an approximation, as it is estimated that only about half of the people with diabetes have been diagnosed. Overall, 80% of known diabetics are over the age of 40, with only 0.05% under the age of 15.
Dentists now know that untreated periodontal disease in diabetic patients progresses very rapidly, often resulting in early tooth loss. In addition, wound healing following tooth extractions is often very slow and ineffective in these individuals. Other problems that may be encountered are abscesses (painful infections), gingivitis with ulcers or sores, and cracks or fissures in the corners of the mouth. In addition, anti-diabetic medications can also cause the patient to have a very dry mouth, which increases the risk of tooth decay.
Patients with type 1 (primary, insulin-dependent) diabetes and patients with the more common type 2 (non-insulin-dependent) diabetes all have three times the risk of periodontitis than people without diabetes. These individuals are also at greater risk of suffering bone loss and experiencing an active and rapid form of the disease. In addition, the presence of unrecognized or untreated periodontitis increases the likelihood that their diabetes will be poorly controlled. Therefore, treating periodontal disease in diabetic patients is crucial, not only to preserve the teeth, but also to help prevent the potential complications of uncontrolled diabetes.
It is important – and encouraging – to realize that a patient with well-controlled diabetes has no greater risk of periodontal disease than a person without diabetes. Therefore, in patients with diabetes, it is essential to ensure that blood sugar levels are well controlled when dealing with periodontal disease, because the better controlled the diabetes, the more effective the periodontal treatment will be.
Diabetes mellitus – a condition in which the body is unable to properly control its sugar levels – is an increasingly common disease in Western countries, affecting at least 5% of the population. This is an approximation, as it is estimated that only about half of the people with diabetes have been diagnosed. Overall, 80% of known diabetics are over the age of 40, with only 0.05% under the age of 15.
Dentists now know that untreated periodontal disease in diabetic patients progresses very rapidly, often resulting in early tooth loss. In addition, wound healing following tooth extractions is often very slow and ineffective in these individuals. Other problems that may be encountered are abscesses (painful infections), gingivitis with ulcers or sores, and cracks or fissures in the corners of the mouth. In addition, anti-diabetic medications can also cause the patient to have a very dry mouth, which increases the risk of tooth decay.
Patients with type 1 (primary, insulin-dependent) diabetes and patients with the more common type 2 (non-insulin-dependent) diabetes all have three times the risk of periodontitis than people without diabetes. These individuals are also at greater risk of suffering bone loss and experiencing an active and rapid form of the disease. In addition, the presence of unrecognized or untreated periodontitis increases the likelihood that their diabetes will be poorly controlled. Therefore, treating periodontal disease in diabetic patients is crucial, not only to preserve the teeth, but also to help prevent the potential complications of uncontrolled diabetes.
It is important – and encouraging – to realize that a patient with well-controlled diabetes has no greater risk of periodontal disease than a person without diabetes. Therefore, in patients with diabetes, it is essential to ensure that blood sugar levels are well controlled when dealing with periodontal disease, because the better controlled the diabetes, the more effective the periodontal treatment will be.
Before proceeding with an organ transplant, the mouth must be free of periodontal disease and tooth decay. Therefore, it is important to have your dentist examine you prior to surgery so that decisions can be made regarding any necessary treatment in conjunction with your transplant specialist.
After the transplant procedure, you will need to take long-term immunosuppressive therapy to prevent rejection of the organ, which will put you at increased risk for periodontal disease. One of the most commonly used immunosuppressive drugs is cyclosporine A. Blood pressure lowering drugs, such as calcium antagonists, are also often prescribed to transplant patients. In many people, these drugs cause thickening of the gums after a few months of treatment, called gingival hyperplasia, which is more likely to occur if inflammation is already present in the gums. Gingival hyperplasia develops mainly between the teeth as small swellings, but it can also develop into a more generalized bulging of the gums. The invaded gums partially cover the teeth and make it very difficult to remove plaque, which leads to the onset of inflammation.
Before proceeding with an organ transplant, the mouth must be free of periodontal disease and tooth decay. Therefore, it is important to have your dentist examine you prior to surgery so that decisions can be made regarding any necessary treatment in conjunction with your transplant specialist.
After the transplant procedure, you will need to take long-term immunosuppressive therapy to prevent rejection of the organ, which will put you at increased risk for periodontal disease. One of the most commonly used immunosuppressive drugs is cyclosporine A. Blood pressure lowering drugs, such as calcium antagonists, are also often prescribed to transplant patients. In many people, these drugs cause thickening of the gums after a few months of treatment, called gingival hyperplasia, which is more likely to occur if inflammation is already present in the gums. Gingival hyperplasia develops mainly between the teeth as small swellings, but it can also develop into a more generalized bulging of the gums. The invaded gums partially cover the teeth and make it very difficult to remove plaque, which leads to the onset of inflammation.

Using phenytoin for epilepsy
If you need to take phenytoin to control your epilepsy, read on to learn how your medication may put you at risk for periodontal disease and what you can do about it.
Phenytoin is an anticonvulsant drug, which is sometimes used to treat epilepsy. In some people, it causes overgrowth of the gums, making it very difficult to clean the teeth. As a result, bacterial plaque builds up and causes inflammatory changes in the gums that lead to gingivitis and, potentially, periodontitis. Gum enlargement is more likely to occur if the patient has poor oral hygiene or if inflammatory changes are already present in the gums at the beginning of treatment.
Using phenytoin for epilepsy
If you need to take phenytoin to control your epilepsy, read on to learn how your medication may put you at risk for periodontal disease and what you can do about it.
Phenytoin is an anticonvulsant drug, which is sometimes used to treat epilepsy. In some people, it causes overgrowth of the gums, making it very difficult to clean the teeth. As a result, bacterial plaque builds up and causes inflammatory changes in the gums that lead to gingivitis and, potentially, periodontitis. Gum enlargement is more likely to occur if the patient has poor oral hygiene or if inflammatory changes are already present in the gums at the beginning of treatment.
Contact us, we are at your disposal
You can write to us to request an appointment, to obtain information or to leave us a comment or advice to improve our services and the reception of our patients.
Cabinet Dentaire de Nyon
Telephone: 022 361 33 00
Address: Rue de la Gare, 11, 1260, Nyon
Mail: info@CabinetDentaireNyon.ch
The office is easily accessible:
By car, with parking spaces available within the building (Parking Bel Air) and 2 parking lots within 300 meters (parking Perdtemps, parking de la Gare)
By public transport: 2.5 minutes walk from the Nyon train station
